|
|
|
Indian Pediatr 2011;48: 325-328 |
 |
MRI Abnormalities of the Anterior Temporal
Lobe: A New Indicator of Congenital Cytomegalovirus Infection |
|
Mahesh Kamate, Manisha Bhandankar, SM Dhaded, *Virupaxi Hattiholi
From the Departments of Pediatrics and *Radiology, KLE
University’s J N Medical College, Belgaum, Karnataka, India.
Correspondence to: Dr Mahesh Kamate, Assistant Professor
of Paediatrics, KLE University’s J N Medical College, Belgaum 590 010,
Karnataka State, India.
Email: [email protected]
Received: August 07, 2009;
Initial review: November 23, 2009;
Accepted: January 4, 2010.
|
Abnormalities of the anterior part of the temporal lobe (abnormal and
swollen white matter, cysts, and focal enlargement of the anterior part
of the inferior horn- either alone or more often in combination) suggest
congenital cytomegalovirus (CMV) infection. This is not widely known.
These can be seen in neonatal period and they continue to persist in
later life.
Key words: Cytomegalovirus, Neonate, Temporal lobe.
|
|
C
ytomegalovirus (CMV) is the
leading cause of congenital infections and in the West, it affects
about 1% of all live births
[1]. Intrauterine CMV infection presents in the neonatal period as
jaundice, hepatosplenomegaly, petechiae, microcephaly, and
chorioretinitis. At the same time, it is also known that about 90%
of infants affected by intrauterine CMV infection are asymptomatic
at birth [1,2]. Serological tests for diagnosing congenital CMV
infection are not very sensitive [3].
With the wider availability of MRI, it has become
the neuroimaging modality of choice for evaluating neurological
conditions in newborn and infants. It is important to note that
unless particular sequences are used, calcifications are commonly
missed on MRI. Periventricular calcifications on computed tomography
(CT) scan of brain always used to be clue for congenital infections.
Abnormalities of the anterior part of the temporal lobe (abnormal
and swollen white matter, cysts, and focal enlargement of the
anterior part of the inferior horn-either alone or more often in
combination) can suggest CMV infection [4]. The present case
highlights this fact.
Case Report
A full-term baby was born out of an uneventful
pregnancy to a non-consanguineously married couple. On day 4 of
life, mother noticed jaundice but baby continued to remain well. The
stools were yellowish in colour and urine high coloured. On day 10
of life, baby was referred with history of melena and hemetemesis.
On examination, vitals were stable but baby had continuous cyclical
movements of all 4 limbs with intermittent shrill cry. Per abdomen
examination revealed a firm enlarged liver (span 10 cm) and mild
splenomegaly. There was no evidence of any rash or petechiae or
purpura. Other systemic examination was within normal limits.
This baby was born to a fourth gravida mother
with no living issues. She had two still- births after the first
pregnancy for which she was investigated. IgG anti-CMV antibodies
were raised when tested in the mother four weeks prior to
conception. No further interventions had been done in the mother.
Investigations revealed a prolonged coagulation
time and thrombocytopenia with hyponatremia. Cerebrospinal fluid
examination was normal as were the renal function tests. There was
conjugated hyperbilirubinemia (total-12 mg/dL; direct-8.1 mg/dL)
with raised liver enzymes. TORCH serology was negative in the baby
and fundus examination did not show any evidence of chorioretinitis.
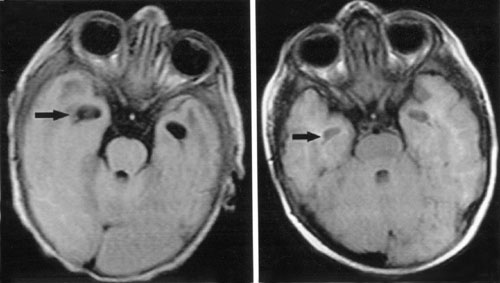
Magnetic resonance imaging (MRI) of brain showed signal changes in
right parieto-occipital region that were hypointense on T1W image
and hyperintense on T2W images. Incidentally, cystic lesions were
noted in bilateral temporal lobes anteriorly (Fig 1a).
These cystic lesions prompted us to send blood for CMV DNA PCR
studies which came positive thereby confirming the diagnosis of
congenital CMV infection. Later a plain CT scan of head was done
which revealed bilateral periventricular calcification suggesting
CMV infection.
 |
|
(a) |
(b) |
|
Fig 1 (a) MRI findings (FLAIR
image axial section) on day 15 showing symmetrical cystic
lesions in the anterior temporal white matter (arrow), (b)
Follow up scan after 9 months (FLAIR image axial section)
shows persistence of cystic lesions in the anterior temporal
white matter (arrow). |
Hyponatremia was corrected slowly over 48-hours
and convulsions were controlled with phenobarbitone. Injection
ganciclovir was given for four weeks with careful monitoring of the
blood counts and liver function tests. Baby received packed cell
transfusion twice during gancyclovir therapy. There were no episodes
of thrombocytopenia or granulocytopenia. Brain-stem evoked response
audiometry done at six weeks of life revealed elevated threshold on
left side and normal threshold on right side. Early intervention
program was advised to parents.
The baby was on regular monthly follow-up and at
one year of age, child has normal developmental milestones. There
was no recurrence of seizures or any neuro-deficits. Repeat MRI at
one year showed the persistence of the anterior temporal horn cysts.
Rest of the brain parenchyma was normal (Fig. 1b).
Discussion
Congenital CMV infection is one of the leading
causes of mental deficiency [1,2]. Serological diagnosis is not fool
proof and is complicated by the maternal transfer of IgG antibodies
and ineffective production of IgM antibodies by the neonate [3].
More sensitive and specific studies like CMV DNA PCR studies are not
widely available in most places, especially in developing countries.
If diagnosed at birth, early initiation of gancyclovir (< one-month
of age) can prevent future development of deafness in the neonate)
[5]. There is a need for some more sensitive and specific tests or
markers which are widely available and can diagnose CMV infection.
Neuroimaging is one such test [4].
There are many reports of abnormalities on CT
scan of brain in congenital CMV infection. In neonatally symptomatic
patients, frequent findings include intracranial calcifications,
ventriculomegaly, white matter abnormalities, neuronal migration
abnormalities, and an extensive destructive encephalopathy [6-8].
In 20%-30% of patients, CT scan can be normal [6,7]. In asymptomatic
patients, Williamson, et al. [9] observed white matter
abnormalities in only 14% of the children.
Studies describing MR imaging findings in
congenital CMV infection when compared to CT scan have been very
less [4]. The MRI findings in
symptomatic infections include dilated ventricles, enlarged
subarachnoid spaces, gyral abnormalities like polymicrogyria,
delayed myelination, and deep white matter lesions mainly in
parietal area. Cysts in the anterior portion of the temporal lobe
and dilated inferior horns in patients with CMV infection were
reported by Barkovich and Lindan [10].
Abnormalities of the anterior part of the
temporal lobe, including abnormal and swollen white matter, cysts,
and focal enlargement of the anterior part of the inferior horn -
either alone or more often in combination appear to be particularly
suggestive of congenital CMV infection. In a study by van der Knaap
MS, et al. [4], amongst all the neuroimaging findings,
abnormalities of the anterior part of the temporal lobe emerged as
the most optimal predicting variable for congenital CMV infection
[4]. In their study, 94% of patients with anterior temporal lobe
abnormalities showed positive results on culture or PCR studies for
CMV infection.
The present case report highlights how specific
neuroimaging findings like anterior temporal horn cysts in a neonate
may suggest a possibility of CMV infection. It also demonstrates
that these changes continue to persist later in life and can be seen
even in neurologically normal patients.
Contributors: MB diagnosed the condition in
the patient and was involved in the management of the case. MK has
drafted the article and will act as the guarantor of the manuscript.
SD did the literature search. VH reported the neuroimaging findings
and reviewed the literature.
Funding: None.
Competing interests: None stated.
References
1. Demmler GJ. Summary of a workshop on
surveillance for congenital cytomegalovirus disease. Rev Infect Dis.
1991;13:315-29.
2. Istas AS, Demmler GJ, Dobbins JG, Stewart JA.
Surveillance for congenital cytomegalovirus disease: a report from
the National Congenital Cytomegalovirus Disease Registry. Clin
Infect Dis. 1995;20:665-70.
3. Brown H, Abernathy M. Cytomegalovirus
infection. Seminars in Perinatology. 1998;22:260-6.
4. van der Knaap MS, Barkhof GVF, Hart AAM,
Loeber JG, Weel JFL. MR Imaging Findings in congenital
cytomegalovirus infection. Radiology. 2004;230: 519-36.
5. Whitley RJ, Cloud G, Gruber W, Storch GA,
Demmler GJ, Jacobs RF, et al. Ganciclovir treatment of
symptomatic congenital cytomegalovirus infection: results of a phase
II study. National Institute of Allergy and Infectious Diseases
Collaborative Antiviral Study Group. J Infectious Disease.
1997;175:1080-6.
6. Noyola DE, Demmler GJ, Nelson CT, Griesser C,
Williamson WD, Atkins JT, et al. Early predictors of
neurodevelopmental outcome in symptomatic congenital cytomegalovirus
infection. J Pediatr. 2001;138:325-31.
7. Boppana SB, Fowler KB, Vaid Y, Hedlund G,
Stagno S, Britt WJ, et al. Neuroradiographic findings in the
newborn period and long-term outcome in children with symptomatic
congenital cytomegalovirus infection. Pediatrics. 1997; 99:409-14.
8. Bale JF, Bray PF, Bell WE. Neuroradiographic
abnormalities in congenital cytomegalovirus infection. Pediatr
Neurol. 1985;1:42-7.
9. Williamson WD, Percy AK, Yow MD, Gerson P,
Catlin FI, Koppelman ML. Asymptomatic congenital cytomegalo-virus
infection. Audiologic, neuroradiologic, and neurodevelopmental
abnormalities during the first year. Am J Dis Child.
1990;144:1365-8.
10. Barkovich AJ, Lindan CE. Congenital
cytomegalovirus infection of the brain: imaging analysis and
embryological considerations. AJNR Am J Neuroradiol. 1994;15:
703-15.
|
|
|
 |
|

